MON : 10 AM – 8 PM
TUE : 10 AM – 7 PM
WED : 10 AM – 8 PM
THU : 10 AM – 6 PM
FRI : 10 AM – 6 PM
SAT : 10 AM – 5 PM
SUN : CLOSED
*We are closed on all public holidays
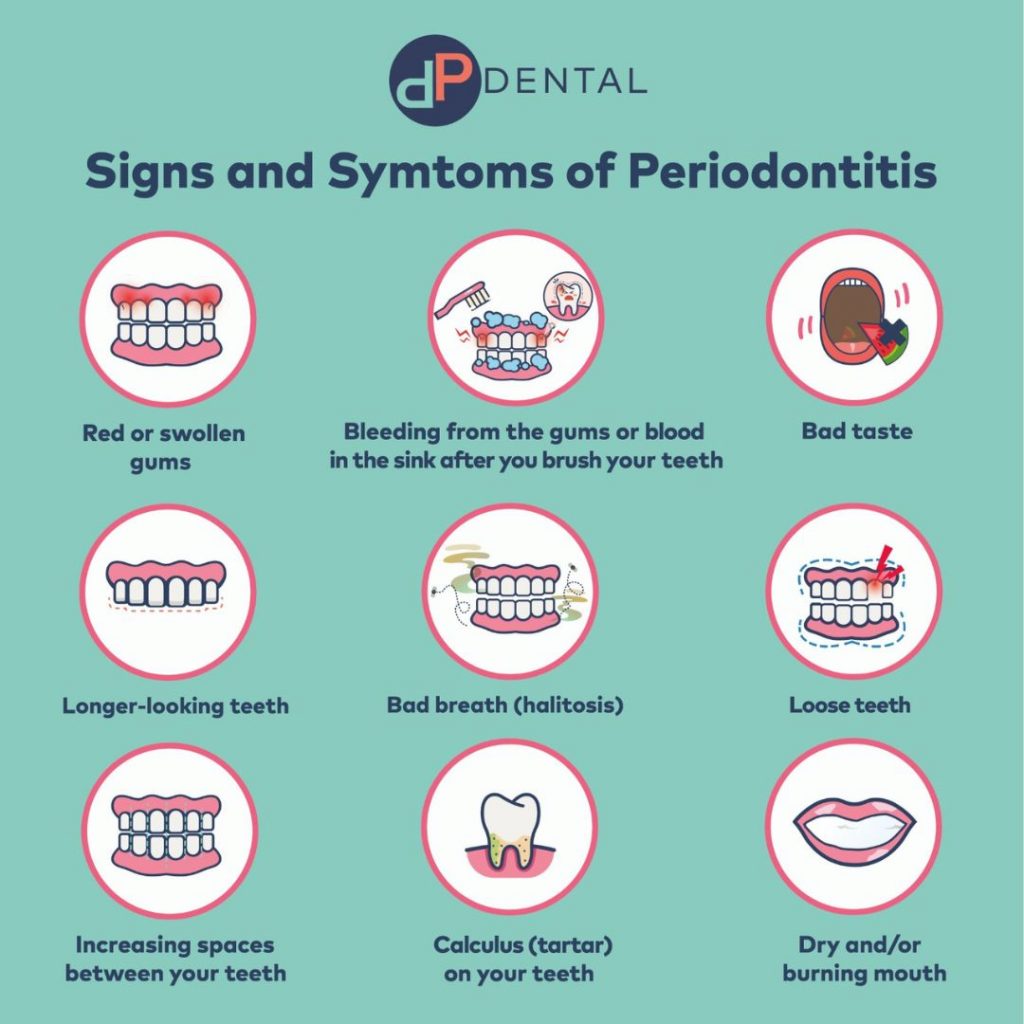
Though it is possible to have gum disease without any symptoms, most patients suffering from periodontal disease do exhibit one or more of the following symptoms:




We operate three clinics in Kovan, Orchard and Katong. Each clinic is equipped with modern technology and is easily accessible by public transport.

Instead of dealing with gum disease after it happens, our oral biofilm screening at DP Dental lets us prevent issues proactively. We identify problems at the root cause, allowing us to create personalised treatment plans based on your unique oral microbiome for precise and effective care.

Erbium lasers offer a minimally invasive solution to periodontal disease, blending efficiency with patient comfort. DP Dental, at the forefront of this technology since 2008, employs highly experienced clinicians proficient in using the Biolase Waterlase iPlus and Fotona LightWalker systems. These advanced tools allow for precise removal of diseased tissue, reduced bacterial and viral load and promote the healing of healthy tissue, significantly improving treatment outcomes.
We operate three clinics in Kovan, Orchard and Katong. Each clinic is equipped with modern technology and is easily accessible by public transport.
Instead of dealing with gum disease after it happens, our oral biofilm screening at DP Dental lets us prevent issues proactively. We identify problems at the root cause, allowing us to create personalised treatment plans based on your unique oral microbiome for precise and effective care.
At DP Dental, we offer laser treatment (using the BIOLASE Waterlase system) for gum disease which is highly effective in gum disinfection and killing bacteria. Our laser treatment for gum disease is minimally invasive, involves less bleeding, pain and swelling, and promotes faster healing.
Periodontal diseases, such as gingivitis and periodontitis, are the most prevalent inflammatory diseases among humans. Periodontitis, the more severe form, damages the gums, bones, and supporting tissues of the teeth. It is triggered by pathogens in dental plaque, both above and below the gum line.
Left untreated, periodontitis can lead to tooth loss, impacting eating, speaking, smile aesthetics, and lowered self-confidence and quality of life. Periodontitis is associated not only with an increased risk of diabetes but also with other conditions, including cardiovascular disease, Alzheimer’s disease, certain cancers, complications during pregnancy, and erectile dysfunction.
Diabetes mellitus, commonly known as diabetes, is characterised by high blood sugar levels (hyperglycemia) and has two major forms. Type 1 diabetes results from a lack of insulin due to an autoimmune reaction in the pancreas, while type 2 diabetes occurs due to insulin resistance linked to chronically high blood sugar levels.
Long-term high blood sugar levels can damage blood vessels, increasing the risk of heart attacks, strokes, eye problems, kidney problems, and foot problems that can result in amputation.
Periodontitis and diabetes have a bidirectional relationship. Healthy individuals with periodontitis are more likely to develop pre-diabetes and diabetes, while severe periodontitis increases the risk of developing type 2 diabetes. Periodontitis is linked to poorer glycemic control and higher blood glucose levels in both diabetic and non-diabetic individuals. Successful periodontal treatment may improve diabetes outcomes.
If you have diabetes, schedule a dental appointment, informing your dentist of diabetes control results and any medication changes. Even without gum disease, regular dental check-ups and good oral hygiene practices are essential for diabetes management. At DP Dental, we can assess your risk for systemic infection due to the presence of certain bacteria, and recommend suitable interventions tailored to your level of risk and condition. This risk assessment helps identify specific pathogens in your oral microbiome before they impact your health.
Managing diabetes becomes more complex with coexisting periodontitis. Individuals with both conditions face a higher risk of severe medical complications, including heart disease, chronic kidney disease, and retinopathy, compared to those with diabetes alone.
